Biallelic cubilin pathogenic variants as a cause of « benign » proteinuria: implications for clinical management
Abstract
The recent description of a cohort with both adults and children harboring biallelic pathogenic variants of CUBN changed the paradigm of the management of isolated proteinuria. Indeed, the detection of proteinuria in a patient, regardless of age, often leads to an exhaustive check-up including kidney biopsy but also the prescription of renin-angiotensin system (RAS) blockers to slow the progression of kidney disease. Patients with CUBN variants have nondetrimental proteinuria and are non-responsive to RAS blockers. We herein describe 2 siblings treated for isolated proteinuria for several years, eventually diagnosed with CUBN biallelic pathogenic variants (c.703 C > T and c.10363-3A > G). We review the physio-pathological mechanisms of this newly discovered disease and discuss implications for clinical management.
Keywords
INTRODUCTION
Discovering isolated proteinuria in a patient should lead to an appropriate work-up, including biological analysis, kidney ultrasound, and, in some cases, kidney biopsy. Proteinuria may be glomerular (mainly albuminuria with or without microscopic hematuria), tubular (low molecular weight proteins such as
CLINICAL CASE
An 8-year-old girl of Turkish origin with no relevant medical history presented to the Pediatric Nephrology clinic for nocturnal enuresis. An initial check-up revealed isolated mild proteinuria (protein/creatinine ratio 1.2 g/g), consisting predominantly of albuminuria. The estimated glomerular filtration rate (eGFR) was normal, as was the ultrasound of the kidneys. A kidney biopsy was performed but it only contained a single glomerulus with a normal appearance by light microscopy. Immunofluorescence was negative. Enalapril was started at 2.5 mg/day. She remained on this medication for 15 years, and proteinuria remained stable at 0.7 g/g to 1.2 g/g despite an increase in enalapril dosage up to 15 mg/day. Enalapril was poorly tolerated, with frequent episodes of orthostatic hypotension. eGFR remained completely normal.
Her younger brother was also found to have moderate isolated proteinuria (0.9 g/g) during a check-up for a hyperactive bladder. His kidney biopsy showed eight normal glomeruli by light microscopy. Immunofluorescence was negative. Enalapril was started, and proteinuria remained stable at 0.6-0.9 g/g over the course of eight years, with preserved eGFR. Both parents have normal urinalysis without proteinuria. The first genetic testing was performed in 2018 in both siblings with a panel including 20 genes related to proteinuria. Results were not contributive, as a single variant of uncertain significance (VUS) of the ACTN4 (actinin alpha 4) gene was found in the sister but not in her brother. Updated genetic testing performed in 2022 [next generation sequencing (NGS) panel enriched for 40 genes important for proteinuric renal diseases][5] revealed in both siblings the presence of a pathogenic nonsense variant [American College of Medical Genetics and Genomics/Association for Molecular Pathology (ACMG/AMP) class 5] together with a potential splice-disrupting variant (ACMG/AMP class 3) in the CUBN (NM_001081.4):c.703 C > T (p.Arg235ter) and c.10363-3A
DISCUSSION
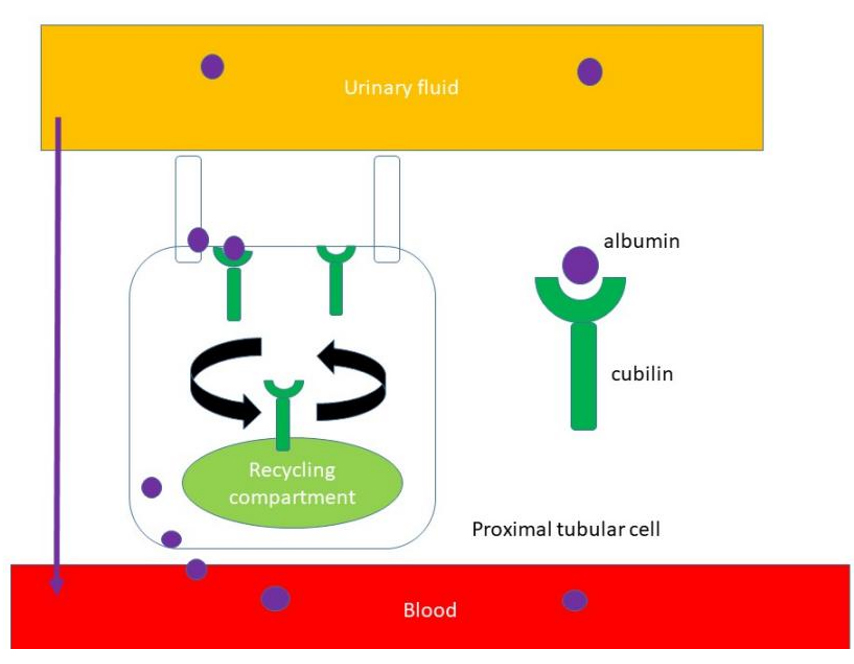
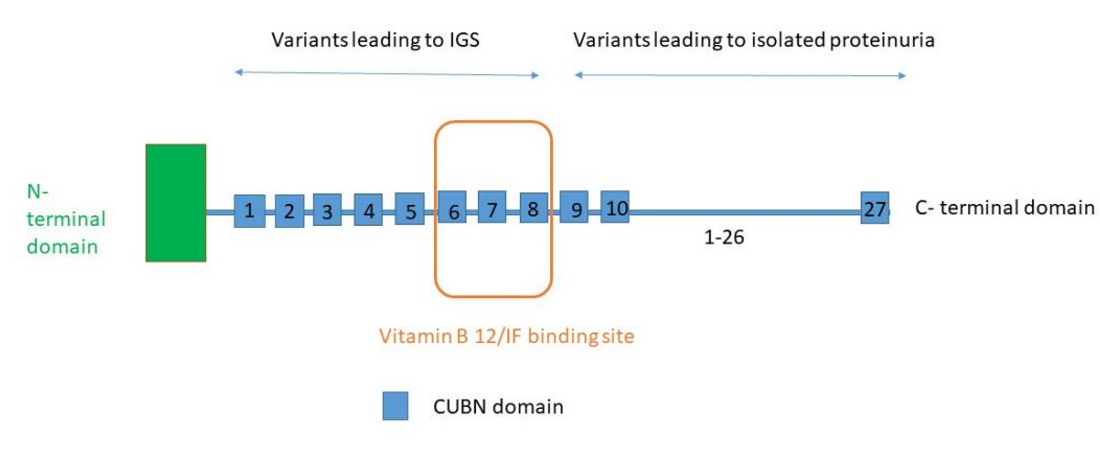
The proximal tubule reabsorbs large amounts of low-molecular-weight proteins but also albumin and electrolytes from the glomerular filtrate. Megalin (LRP2), CUBN, and amnionless (AMN) protein are located in the apical part of proximal tubular cells and are responsible for receptor-mediated endocytosis of proteins filtered through the glomerular barrier[3]. Cubilin has been shown to have an essential role in albumin reabsorption and is encoded by the CUBN gene [Figure 1][6]. Biallelic pathogenic variants in the CUBN gene cause Imerslund-Gräsbeck syndrome (OMIM 261100), also called selective vitamin B12 (cobalamin) malabsorption with proteinuria[6]. In this syndrome, which results in megaloblastic anemia responsive to parenteral vitamin B12 therapy, half of the patients present with mild proteinuria and normal eGFR. The megaloblastic anemia arises from a defect in the receptor for the vitamin B12-intrinsic factor complex in ileal enterocytes. CUBN and AMN proteins represent the two subunits of this receptor. In patients with Imerslund-Gräsbeck syndrome, proteinuria can persist for decades[7,8]. Most pathogenic variants in CUBN are located in the N-terminal half of the gene [Figure 2].
Figure 1. Albumin reabsorption in proximal tubular cells. Cubilin is located in the apical part of proximal tubular cells and is responsible for receptor-mediated endocytosis of albumin filtered through the glomerular barrier. After the decoupling of cubulin-albumin ligation, albumin is released from the basolateral cell surface into the circulation.
Figure 2. Cubilin protein structure. Cubilin (CUBN) is a 460 kDa glycoprotein with no transmembrane domain. It acts as a receptor for intrinsic factor-vitamin B12 complexes. There are 27 CUB domains. The intrinsic factor and the vitamin B12 binding region are located in domains 5 to 8. The precise location of the binding sites for albumin remains unclear, but it is supposed to be in the CUB domains near the C-terminal area. IGS: Imerslund-Grasbëck syndrome; IF: intrinsic factor.
Recently, biallelic pathogenic variants in the C-terminal domain of CUBN were described as leading to isolated chronic proteinuria[4]. Indeed, Bedin et al.[4] identified 39 patients with biallelic CUBN variants among 2,216 individuals with suspected genetic kidney disease, including proteinuric patients. Proteinuria ranged from 0.5-3 g/day with an average age at discovery of 10.9 years. When measured, albuminuria represented more than half of proteinuria, and β2-microglobulin urine levels were low or absent. Kidney biopsies were available in 19 patients and did not show any specific lesion in 11 patients. Four kidney biopsies underwent electron microscopy (EM) evaluation; two were normal and two revealed glomerular synechiae. The use of ACE inhibitors did not lower proteinuria, which remained stable over the years. eGFR was normal in all patients, even those older than 50 years. Bedin et al.[4] also identified a phenotype-genotype correlation. Indeed, variants located after the CUB8 domain (included in the vitamin B12/intrinsic factor binding region) lead to isolated proteinuria, whereas variants located before the CUB8 domain result in Imerslund-Gräsbeck syndrome, a finding suggesting that there are separate binding sites in cubilin for vitamin
In another recent cohort, Domingo-Gallego et al.[14] identified 15 patients with mild proteinuria
In conclusion, in the absence of functional cubilin in proximal tubular cells, albumin reabsorption is incomplete, and this leads to mild albuminuria. This mechanism acts downstream of the glomerular barrier, and does not affect the intraglomerular pressure, and is thus not expected to damage podocytes. This explains why anti-proteinuric agents such as ACE inhibitors do not succeed in lowering this particular proteinuria. Detection of CUBN pathogenic variants is crucial in clinical nephrology because it prevents unnecessary kidney biopsies as well as the use of RAS blockers and their potential side effects, such as symptomatic hypotension or, rarely, angioneurotic edema. The benign course of this disease needs to be confirmed by longer-term follow-up.
DECLARATIONS
Authors’ contributions
Contributed to the concept, design, draft, and revision of this manuscript: Gillion V, Dahan K, Godefroid N
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Ethics approval was deemed unnecessary according to national regulations (i.e., the Belgian law of 7/5/2004 concerning experiments on human subjects). All participants provided written consent to participate in this study.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2023.
REFERENCES
1. Roscioni SS, Lambers Heerspink HJ, de Zeeuw D. Microalbuminuria: target for renoprotective therapy PRO. Kidney Int. 2014;86:40-9.
2. Hemmelgarn BR, Manns BJ, Lloyd A, et al.; Alberta Kidney Disease Network. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303:423-9.
3. Quinlan C. CUBN variants uncouple proteinuria from kidney function. Nat Rev Nephrol. 2020;16:135-6.
4. Bedin M, Boyer O, Servais A, et al. Human C-terminal CUBN variants associate with chronic proteinuria and normal renal function. J Clin Invest. 2020;130:335-44.
5. Knoers N, Antignac C, Bergmann C, et al. Genetic testing in the diagnosis of chronic kidney disease: recommendations for clinical practice. Nephrol Dial Transplant. 2022;37:239-54.
6. Amsellem S, Gburek J, Hamard G, et al. Cubilin is essential for albumin reabsorption in the renal proximal tubule. J Am Soc Nephrol; 2010. 1859-67
7. Gräsbeck R. Imerslund-Gräsbeck syndrome (selective vitamin B12 malabsorption with proteinuria). Orphanet J Rare Dis. 2006;1:17.
8. Aminoff M, Carter JE, Chadwick RB, et al. Mutations in CUBN, encoding the intrinsic factor-vitamin B12 receptor, cubilin, cause hereditary megaloblastic anaemia 1. Nat Genet. 1999;21:309-13.
9. Ahluwalia TS, Schulz CA, Waage J, et al. A novel rare CUBN variant and three additional genes identified in Europeans with and without diabetes: results from an exome-wide association study of albuminuria. Diabetologia. 2019;62:292-305.
10. Böger CA, Chen MH, Tin A, et al.; CKDGen Consortium. CUBN is a gene locus for albuminuria. J Am Soc Nephrol. 2011;22:555-70.
11. Haas ME, Aragam KG, Emdin CA, et al.; International Consortium for Blood Pressure. Genetic association of albuminuria with cardiometabolic disease and blood pressure. Am J Hum Genet. 2018;103:461-73.
12. Zanetti D, Rao A, Gustafsson S, Assimes TL, Montgomery SB, Ingelsson E. Identification of 22 novel loci associated with urinary biomarkers of albumin, sodium, and potassium excretion. Kidney Int. 2019;95:1197-208.
13. Teumer A, Tin A, Sorice R, et al.; DCCT/EDIC. Genome-wide association studies identify genetic loci associated with albuminuria in diabetes. Diabetes. 2016;65:803-17.
14. Domingo-Gallego A, Pybus M, Madariaga L, et al. Clinical and genetic characterization of a cohort of proteinuric patients with biallelic CUBN variants. Nephrol Dial Transplant. 2022;37:1906-15.
15. Cicek N, Alpay H, Guven S, et al. Clinical and genetic characterization of children with cubilin variants. Pediatr Nephrol. 2023;38:1381-5.
16. Yang J, Xu Y, Deng L, et al. CUBN gene mutations may cause focal segmental glomerulosclerosis (FSGS) in children. BMC Nephrol. 2022;23:15.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Copyright
Data & Comments
Data
















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].